A 77-year-old woman with subfoveal classic choroidal neovascularization secondary to AMD.
A: Fundus autofluorescence image.
B: Early phase fluorescein angiogram, and (C) and late-phase (D) fluorescein angiogram. Focal areas of decreased autofluorescence inside the lesion and a rim of increased intensity around the lesion are observed.
Illustration of a newly diagnosed pigment epithelium detachment in the right eye of a 63-year-old man.
A: Fundus photograph.
B: Fundus autofluorescence image.
C: Late-phase fluorescein angiography.
D: Indocynanin-green angiography. There is high-autofluorescent material inside the detachment and the borders of the detachment are clearly delineated by a ring of decreased autofluorescence intensity.
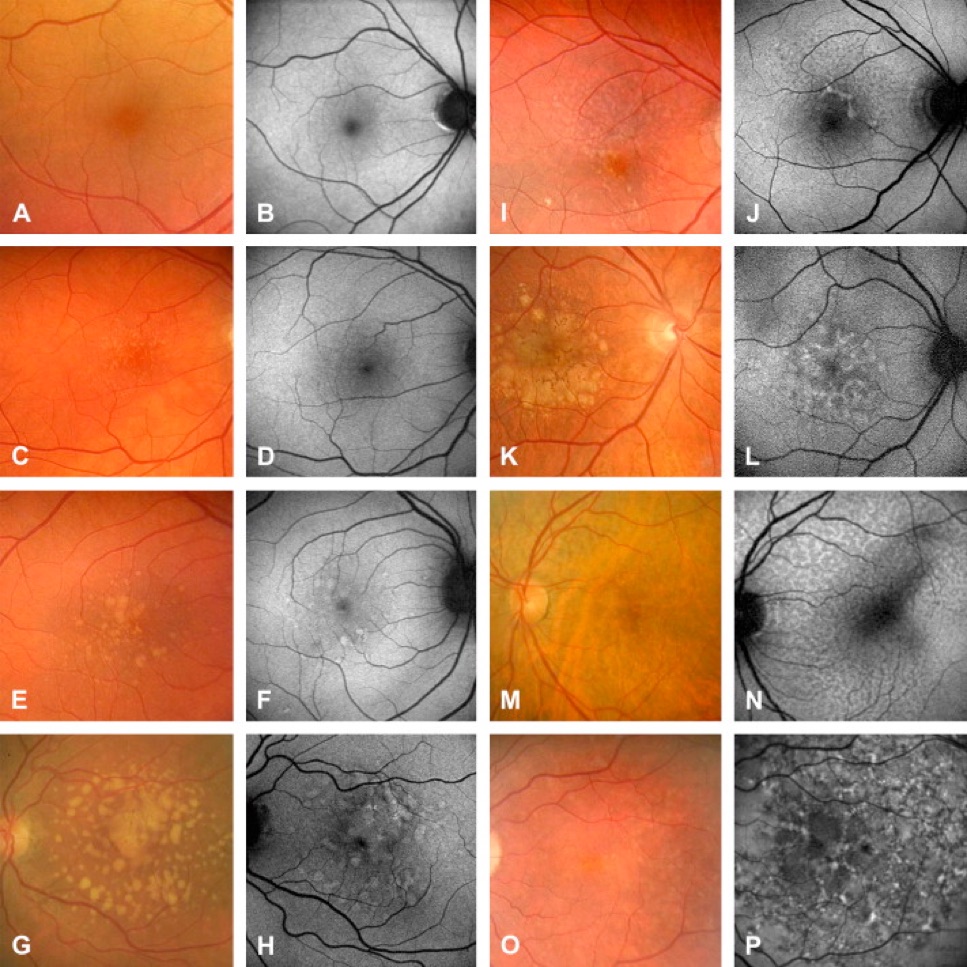
Classification abnormal autofluorescence patterns in early age-related macular disease with fundus photography and autofluorescence images introduced by Bindewald et al.12 Eight phenotypic patterns are differentiated:
NORMAL (A, B) – homogenous background FAF and a gradual decrease in the inner macula toward the fovea due to the masking effect of macular pigment. Only small hard drusen are visible in the corresponding fundus photograph.
MINIMAL CHANGE (C, D) – only minimal variations from normal background FAF. There is limited irregular increase or decrease in FAF intensity due to multiple small hard drusen.
FOCAL (E, F) – several well-definied spots with markedly increased FAF. Fundus photograph of the same eye with multiple including hard and soft drusen.
PATCHY (G, H) – multiple large areas (>200 μm diameter) of increased FAF corresponding to large, soft drusen and/or hyperpigmentation on the fundus photograph
LINEAR (I, J) – characterized by the presence of at least one linear areas with markedly increased FAF. A corresponding hyperpigmented line is visible in the fundus photograph.
LACE-LIKE (K, L) – multiple branching linear structures of increased FAF. This pattern may correspond to hyperpigmentation on the fundus photograph or to no visible abnormalities.
RETICULAR (M, N) – multiple, specific small areas of decreased FAF with brighter lines in-between. The reticular pattern not only occurs in the macular area but is found more typically in a superotemporal location. There may be visible reticular drusen in the corresponding fundus photograph.
SPECKLED (O, P) – variety of FAF abnormalities in a larger area of the FAF image. There seem to be fewer pathologic areas in the corresponding fundus.
Classification of FAF patterns in the junctional zone in patients with geographic atrophy due to AMD. Eyes with no increased FAF intensity at all are graded as “NONE” (= slow progressor). The eyes with increased FAF are divided into two groups depending on the configuration of increased FAF surrounding atrophy.
Eyes showing areas with increased FAF directly adjacent to the margin of the atrophic patch(es) and elsewhere are called ‘diffuse’ (= rapid progressors) and are subdivided in five groups.
From left to right:
(Top row) fine granular, branching, (bottom row) trickling, reticular, and fine granular with punctuated spots.
Eyes with increased FAF only at the margin of GA are split into three subtypes (FOCAL [= slow progressor], BANDED [= rapid progressor], and PATCHY [= no data, occurs rarely]) according to their typical FAF pattern around atrophy.
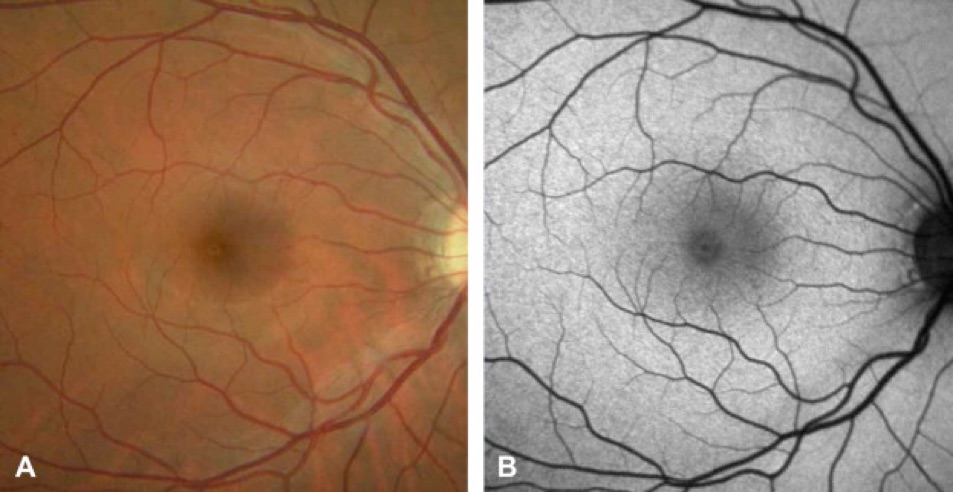
Color fundus photograph (A) and fundus autofluorescence imaging (B) of the right eye in a normal subject with the confocal scanning laser ophthalmoscope (Heidelberg Retina Angiograph, HRA 2, Heidelberg Engineering, Dossenheim, Germany).
Topographical distribution of FAF intensity shows typical background signal with shadows on optic disc (absence of autofluorescent material) and retinal vessels (absorption).
Further, intensity is markedly decreased over the fovea due to the absorption of the blue light by yellow macular pigment.
De Lairessestraat 59 1071 NT Amsterdam 020-679 71 55 omca@me.com www.omca.nl


Amsterdam Eye Hospital
Oogziekenhuis Amsterdam