
Glaucoma patients can present with several types of visual field defects.
However, in most cases progression of visual field defects is parallel to optic nerve head changes.
The first change in the optic nerve head is usually inferior or superior rim tissue thinning that occurs on the inside edge of the rim.
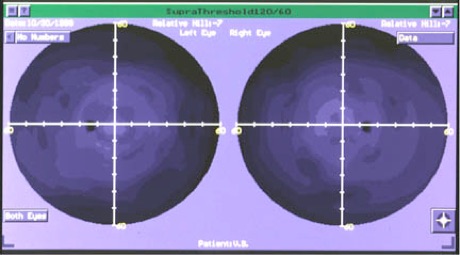
Because the nerve fibers that enter the optic nerve head on the inside edge of the rim originate from areas close to the disc, the earliest visual field changes are seen in the paracentral field, either in the superior or inferior field.
These earliest changes are seen as small areas of depressed sensitivity (relative paracentral scotomas) between 5 and 20 degrees of fixation.
As the rim continues to thin, depressed areas enlarge and deepen circumferentially along the distribution of arcuate nerve fibers (Seidel scotoma) until they coalesce to form an arcuate-shaped defect that joins with the blind spot (Bjerrum or arcuate scotoma).
Because the inferior or superior rim tissue is first involved and then followed by involvement of the opposite rim, double arcuate scotomas can develop.
A nasal step (more loss above or below the horizontal meridian in the nasal field) is frequently associated with paracentral scotomas or arcuate scotomas but may be present by itself.
A temporal wedge defect (temporal to blind spot) may appear. Field loss gradually spreads to periphery and also centrally.
Eventually only a small island of central vision and a temporal “sliver” are left.
Overall generalized depression of sensitivity may also be an indicator, although this is not definitive for glaucoma. Since anatomically nerve fibers do not cross the horizontal raphe, glaucomatous field defects tend to obey the horizontal midline. This is in contrast to post-chiasmal field defects, which tend to obey the vertical midline.
The classic kinetic target Goldman bowl perimeter has been for the most part replaced by numerous automated computer-driven perimeters from several companies (e.g. Dicon, Synemed, Interzeag, Oculus, Medmont, etc.).
Visual field analyzers (L-R) Goldman Bowl, Dicon, Oculus, Humphrey

FASTPAC - Speeds exam using age-reference statistics.
Blue-on-Yellow or SWAP (Short Wave Automated Perimetry) - Uses blue stimuli on yellow background, which isolates blue receptors on
the retina, potentially revealing visual field defects years before defects are found using traditional white stimuli on white background.
Swedish Interactive Testing Algorithm (SITA-Standard, SITA-Fast) - “Smart” program using real-time threshold adjustments to speed
test without data compromise.
Kinetic Goldmann Bowl Perimetry - Mimics kinetic isopter Goldmann Bowl Perimeter.
Glaucoma Progression Analysis - Uses extensive statistical data from glaucoma and normal populations to monitor progression.
The Humphrey/Welch-Allyn Frequency-Doubling Technology (FDT) Perimeter utilizes the frequency-doubling principle to help diagnose visual field loss caused by glaucoma. A stimulus is presented that consists of alternating low spatial frequency black-white grating bars creating. The flicker effect produced by this stimulus isolates M (Magnocellular) cells in the retina and their large diameter neurons. These large neurons may be the first to die in glaucoma.
Good correlation was seen between FDT visual fields and traditional white stimulus on white background threshold visual field tests. The Humphrey Matrix is a newer field analyzer that works on the same principle as FDT, but provides a larger visual field area (same size as a 30-2 threshold test) with the same test points as a 30-2 threshold test.

Various confounding elements may cause misinterpretation of visual field results.
These confounds can include: ptosis, patient fatigue, small pupils, poor alignment, trial lens holder artifacts and other diseases creating glaucoma-like patterns (e.g., retinal vascular occlusions, optic neuropathies, retinal scarring, and strokes).
Patients with early glaucomatous field loss often show variability or fluctuation of fields within a single test session and/or from session to session. Some patients give unreliable visual fields some of the time, while others give unreliable results all of the time.
Multiple measurement attempts may be necessary to confirm field loss. The OHTS results suggested that to get a good baseline visual field, at least two fields taken about two weeks apart are necessary. If the fields do not show similar results, a third visual field taken several months later is useful.
The automation of field testing has not eliminated the need for a skilled technician to be present during testing. The more skillful the technician, the less likely the field will be unreliable. It is necessary to ensure that the patient is properly occluded (to eliminate false positives), that the patient is looking through the appropriate trial lens (to reduce chances of false field loss or generalized sensitivity reduction), and to be sure that the trial lens is as close to the patient's eye and as well-centered as possible to prevent false arcuate scotoma artifacts. The technician must also help the patient retain fixation because excessive loss of fixation makes the visual field invalid.
Fundus Photography
Fundus photography is a common procedure used in the management of glaucoma. Stereo white-light photos are standard, with photos taken at least every two years (or more frequently if changes are noted). Red-free imaging of the nerve fiber layer is also an option. Photography can be used as adjunct to detailed stereoscopic ophthalmoscopic evaluation of the optic nerve and nerve fiber layer. Digital photographic options are now available and can be coupled with computer analysis to quantify retinal features.
Extended Ophthalmoscopy
The doctor may follow glaucomatous progression with dilated fundus evaluations, examining the optic nerve, vasculature, and nerve fiber layer for changes. This examination is independent of the initial eye exam, and requires detailed diagrammatic documentation.
De Lairessestraat 59 1071 NT Amsterdam 020-679 71 55 omca@me.com www.omca.nl


Amsterdam Eye Hospital
Oogziekenhuis Amsterdam

