Signs and symptoms
Terrien's marginal degeneration produces superior nasal peripheral corneal thinning, leaving the epithelium intact. The condition is often bilateral and may occur at any age, although it typically occurs in middle-aged males.
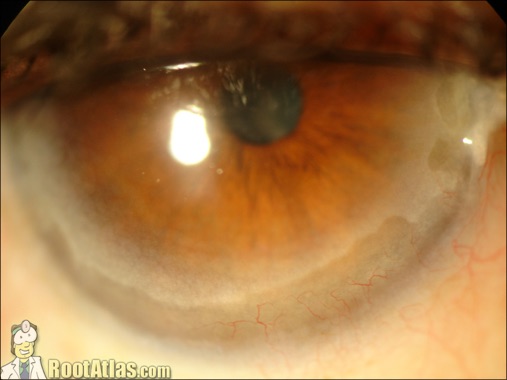
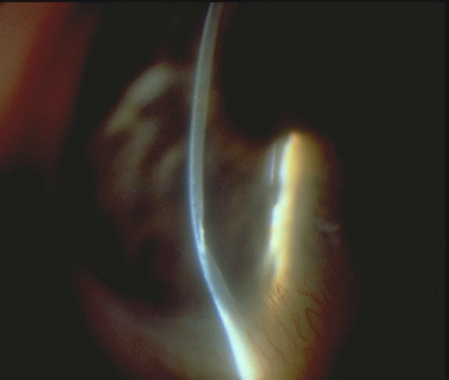
The disease first presents as a peripheral corneal haze. Over time it exhibits a slowly progressive peripheral corneal thinning with a sloping central edge that spares the limbus.
The eyes are typically not injected and there is little if any pain, photophobia or anterior chamber reaction. In fact, aside from increased regular and irregular astigmatism, which may produce visual changes, patients are often asymptomatic.
Physical signs include an interior circumferential, yellow demarcation line composed of lipid and a fine pannus, which may resemble a pterygium.
The degeneration often progresses in a circumferential pattern. Perforation is usually only a complication of trauma. Hydrops can occur in severe cases. A recent report cited a potential association with the chronic, inflammatory skin condition erythema elevatum diutinum (a rash that appears on the buttocks, wrists, elbows and knees).
Pathophysiology
The etiology of Terrien's marginal degeneration is poorly understood.
Histopathologically, the principle findings include fibrosis, vascularization and phagocytosis of corneal stromal collagen by histiocytes, with evidence of increased lysosomal activity.
A local absence of Bowman's membrane characterizes the condition; some cases involve breaks in Descemet's membrane. Autoimmune mechanisms are also potential etiological factors.
Management
Because most patients remain asymptomatic, management of Terrien's marginal degeneration is largely supportive. Terrien's patients may suffer from periodic episodes of red, irritated eyes secondary to mild adjacent conjunctival inflammation.
These cases often respond quickly to topical steroidal medications such as prednisolone acetate 0.12% or 1%, or Lotemax (loteprednol 0.5%) qid.
In cases involving visual symptoms, an astigmatic spectacle correction may be in order. Also, given the risk of corneal perforation from blunt trauma, prescribing ANSI-standard safety glasses is prudent. Polycarbonate lenses are mandatory.
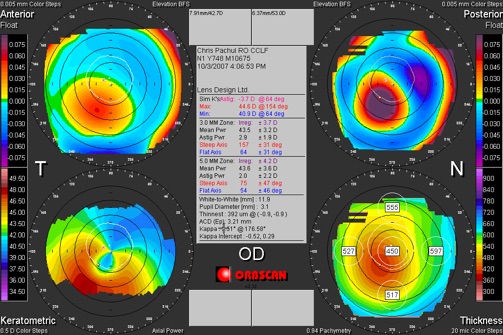
Contact lenses are a plausible modality for restoring vision; however, because of complex, irregular astigmatism the fitting is frequently complex as well, calling for a soft bandage lens with an RGP piggyback.
If you attempt a contact lens correction, also prescribe plano polycarbonate spectacles for safety. When vision is uncorrectable or the risk of perforation is high, consider surgical options--annular full-thickness penetrating keratoplasty, lamellar penetrating keratoplasty or large eccentric corneal grafts.
Clinical Pearls
-
•The differential diagnosis of peripheral corneal thinning includes
-
•peripheral corneal melt secondary to collagen vascular diseases such as rheumatoid arthritis and polyarteritis nodosa (bilateral, typically painful and progressive to perforation)
-
•Mooren's ulceration (unilateral or bilateral, painful corneal thinning with neovascularization)
-
•pellucid marginal degeneration (painless, inferior, peripheral corneal thinning, a variant of keratoconus)
-
•furrow degeneration (painless, peripheral corneal thinning, adjacent to corneal arcus, without vascularization)
-
•dellen (painless, oval thinning secondary to corneal drying)
-
•marginal keratitis secondary to Staphylococcus hypersensitivity (painful, infiltrate present, inset from limbus).
-
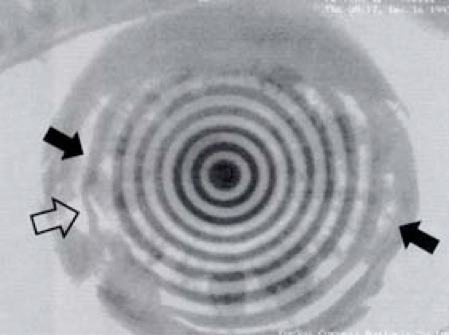
•Topography can help in diagnosing Terrien's marginal degeneration, which exhibits these three features: corneal flattening at the juncture of the furrow; corneal steepening 90 degrees from the flattened area; and a relatively spherical and regular central area.
De Lairessestraat 59 1071 NT Amsterdam 020-679 71 55 omca@me.com www.omca.nl
Amsterdam


Amsterdam Eye Hospital
Oogziekenhuis Amsterdam

