Artificial Vision: Argus II Electronic Epiretinal Implant
Professor Paulo E. Stanga has set-up and is Principal Investigator for a Manchester-only Pilot Study of the Argus II system in Age Related Macular Degeneration (AMD) and has already successfully carried out the first ever implantation of an electronic retinal implant in AMD, which has resulted in the first ever person with integrated artificial (central) and natural (peripheral) vision.
Since early 2009 Professor Stanga and his team have contributed to the advancement of the study through their ongoing research with the enrolled patients. Testing and training with shapes, letters, and short words are helping people to better identify those things which were once so familiar to them. For many of these people, who have gradually lost their sight over time, the brain needs to learn how to recognise the various images that the system sends. Real-world tasks such as the identification of moving/stationary cars or bus stop poles, finding doors and windows, following a crosswalk across the street, localising light sources, and sorting dark/light laundry are also being addressed by the team.
The implant is an epiretinal prosthesis that includes a receiving coil, an electronics package and an electrode array that are surgically implanted in and around the eye.
The entire Argus II system collects video data and wirelessly transmits the signal to the implant. The on-board electronics drive appropriate currents to each electrode in the array and the electrodes then stimulate remaining viable cells in the inner retina. This is intended to produce the perception of spots of light that provide some useful vision.
The external components include glasses, a video processing unit (VPU) and a cable.
The glasses include a miniature video camera, which captures video images, and a coil that sends data and stimulation commands to the implant. The VPU converts the video images into stimulation commands and is worn on the body while the cable connects the glasses to the VPU.
This is the world’s first and only CE mark and FDA approved retinal prosthesis for the blind indicated for severe and profound outer retinal degeneration. Although this is not yet available in the NHS, it is available in the independent/private sector. Please contact Professor Stanga's secretary on 0(+44)1625 581781 for further information.
http://www.retinaspecialist.co.uk/conditions/electronic-retinal-implants/
De Lairessestraat 59 1071 NT Amsterdam 020-679 71 55 omca@me.com www.omca.nl
Diseases like retinitis pigmentosa (RP) are distinguished by the fact that a large part of the retina remains functional even after loss of sight.
Although the rods and cones that normally convert light into nerve signals are destroyed by this disease, most of the retinal nerve tissue, which has the task of pre-processing information on its way to the brain, remains intact.
In other words, the visual apparatus is functional; it just lacks input.
Based on this concept, Eberhart Zrenner at the University Eye Clinic of Tübingen has developed a subretinal implant in cooperation with that university’s Institute of Natural Science and Medicine (NMI).
For the subretinal implant, natural optical stimulus is simply replaced by pulsed, lightdependent electrical stimuli, resulting in the perception of phosphenes (artificially triggered light phenomena). Because the electrical excitation invariably involves a number of cells, the patients cannot visualize objects sharply, but are nevertheless able to locate light sources and localize physical objects.
The implant is located subretinally, i.e. behind the retina.
From an anatomical point of view, it exactly replaces the photoreceptors that have been lost (● see Figure 1). From the viewpoint of signal processing, this is an all-important advantage; the implant’s subretinal excitation exploits the full range of neuronal circuitry in the retina along the way to the optic nerve. The electrical signal is triggered at the point of brightness, and the stimulation strength corresponds to the intensity of the incident light. The optical image is thus exactly replaced by an electrical pattern of excitation.
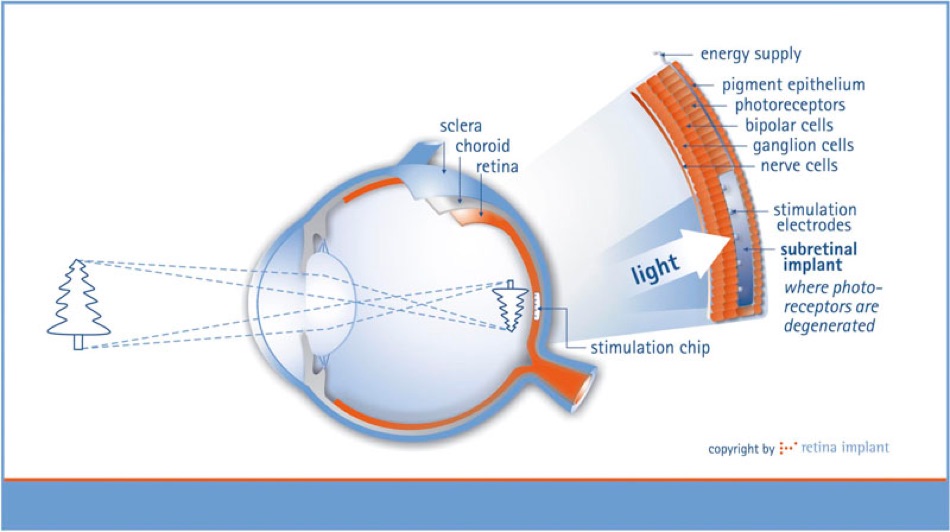
Figure 1) To restore useful visual cues to patients suffering from hereditary retinitis pigmentosa, the subretinal chip replaces the degenerated photoreceptors.
The retinal implant consists of a silicon chip about 3 × 3 mm in size and 70-μm thick, with 1500 individual pixels.
Each of these pixel cells contains a light-sensitive photodiode, a logarithmic differential amplifier, and a 50 × 50-μm iridium electrode into which the electrical stimuli at the retina are guided. The circuitry was developed in collaboration with the IMS in Stuttgart and is made by applying 0.8-μm CMOS technology.
The result is a pure analog chip, with the advantage that its power consumption is very low (maximum 10 mW), and the heat passed on to the retina by electrical power from the chip remains below 0.5 K.
The microchip is positioned on a thin, highly flexible circuit board of polyimide with gold circuits that transmit power and control signals (● See Figure 2). The very fine polyimide strip is connected in turn to a thin, coiled cable through which the electricity of the chip is supplied. This elastic cable passes through the orbital cavity to the bone of the temple and from there to a point behind the ear, where it is connected to an inductive power supply unit in a ceramic housing.
The electrical energy is received inductively from the outside through a second coil that is located on the skin. Permanent magnets in the two coils ensure close contact.
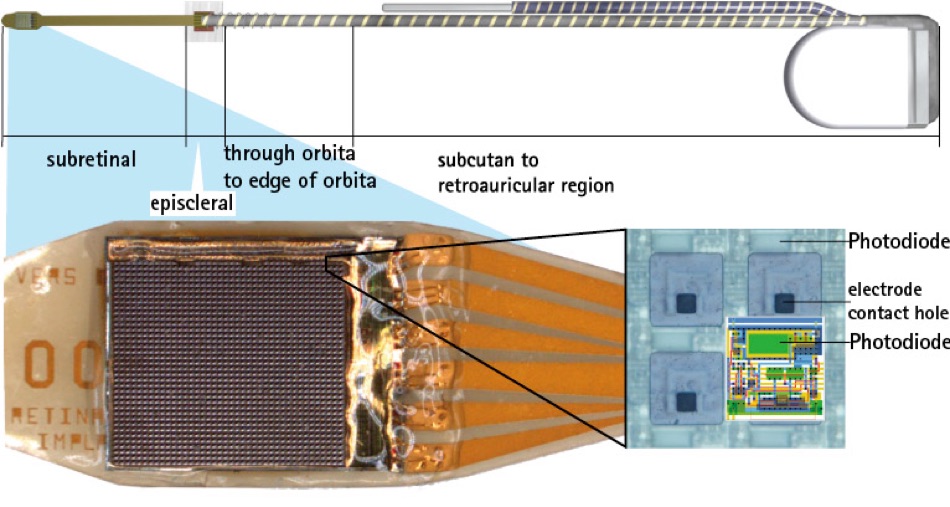
Figure 2) A complementary metal-oxide-semiconductor (CMOS) camera chip rests on a polyimide carrier, and is connected via a silicone cable to a wireless power receiver.
All of the components must of course be biocompatible—that is, well tolerated by the body—and must possess long-term stability. This is an enormous technological challenge that requires, among other things, the use and combination of new materials. The components must be provided with a hermetically sealed protective layer at the point of contact with the surrounding tissue. They must undergo numerous tests to demonstrate the device’s ability to withstand the corrosive environment within the body. An especially critical point is that the presence of electrical voltage can greatly accelerate the corrosion process. The selection of materials and the manner in which they are processed is critical.
Above all, the electrodes and their contact points on the chip are of decisive importance. The useable electrode surface must be as small as possible but also offer as large a surface as possible to ensure good contact with the retina. For this reason, the electrodes are manufactured of fractal iridium, whereby the materials permit a higher transmission of charges. Optimal visual perception is present when pulse durations are around 1 microsecond and the charge amounts to 2–5 nC per pixel. This corresponds to a voltage of up to 2V. The repetition rate of excitation is normally 5–7 Hz, because higher rates would result in overstimulation of the retina. The patient’s visual perception therefore flickers somewhat.
http://www.retina-implant.de/en/patients/technology/default.aspx
Subretinal Implant Technology

Amsterdam Eye Hospital
Oogziekenhuis Amsterdam

