The MAIA software, with its normative database and statistical analysis module, is designed to identify the normal, age‐related, decrease in sensitivity and differentiate it from the pathological changes associated with macular degenerations and other retinal diseases.
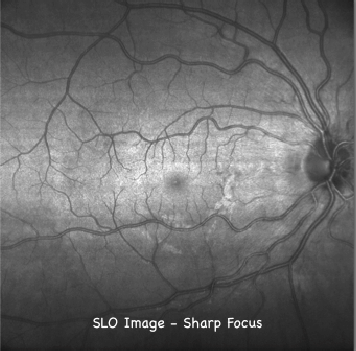
ADVANTAGES OF SLO IMAGING
By using a line scanning laser ophthalmoscope (LSLO) to continuously image the retina, the light reflected by the out‐of‐focus layers does not degrade the quality of the image. The sharp constrast of the SLO image is due to its confocal properties.
EYE TRACKER
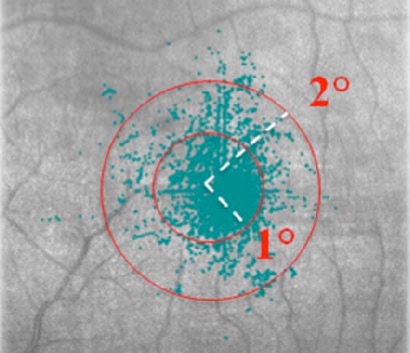
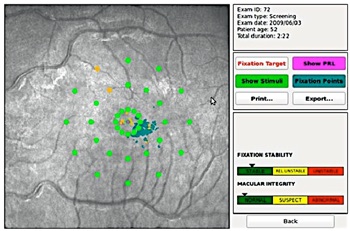
The eye tracker also quantifies a patient’s fixation characteristics: the extent of the area covered by fixation points is a measure of fixation stability, while the location of the gravitational center of the fixation points with respect to the fovea is an indication of fixation location.
These indices aid in the determination of stable, relatively unstable or unstable fixation patterns.
The automated eye tracker is fast, accurate and robust.
It locks onto the entire fundus image and captures fixation changes 25 times per second during testing.
Live images of the retina are processed to “track” anatomical landmarks over the entire image and quantify the corresponding eye movements observed during the test procedure.
MICROPERIMETRY
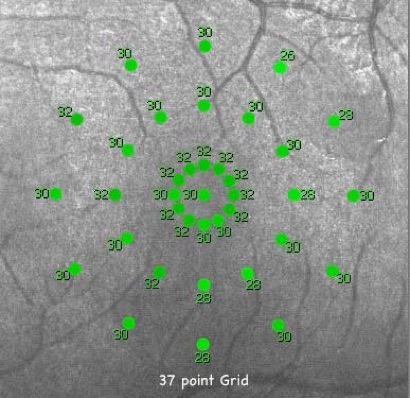
Following eye‐tracking based position corrections, perimetric stimuli are automatically projected in random order using either a supra‐threshold or a 4‐2 threshold strategy to accurately measure macular threshold sensitivity at predefined retinal locations over the central 10° of the retina using a standard Goldmann III stimulus size.
Background luminance is 4 asb; stimulus dynamic range is 36 dB and maximum luminance is 1000 asb. Measured values areaveraged and compared with the age‐adjusted average for normals.
The average macular threshold, along with other variables, serves for the calculation of the macular integrity index, a statistical parameter derived by comparison with normative data that describes the likelihood of threshold values to significantly differ from normal values.
MAIA permits the differentiation of normal age-related loss of macular sensitivity from pathological (disease state) changes that require treatment.
It provides a first step in retinal disease management, enabling us to test macular function and to follow sequential changes of retinal disease and/or treatment over time.
This will allow us to improve our diagnosis and treatment of our patients by detecting disease changes earlier than conventional testing.
De Lairessestraat 59 1071 NT Amsterdam 020-679 71 55 omca@me.com www.omca.nl


Oogziekenhuis OMC Amsterdam
Amsterdam Eye Hospital
De Lairessestraat 59 1071 NT Amsterdam 020-679 71 55 omca@me.com www.omca.nl
Amsterdam


Amsterdam Eye Hospital
Oogziekenhuis Amsterdam