There are two other types of corneal topography printouts clinicians use:
-
•Elevation map.
This utilizes yet another algorithm to give additional information about the cornea. An elevation map shows the measured height from which the corneal curvature varies (above or below) from a computer-generated reference surface. Warm colors depict points that are higher than the reference surface; cool colors designate lower points.
-
• Refractive map.
This utilizes the measured dioptric power and applies Snell's law to describe the cornea's actual refractive power. A refractive map compensates for spherical aberrations as well as the aspheric contour of the cornea. The central portion of the refractive map is most important. This area overlies the pupil, so aberrations here almost invariably impact visual performance.
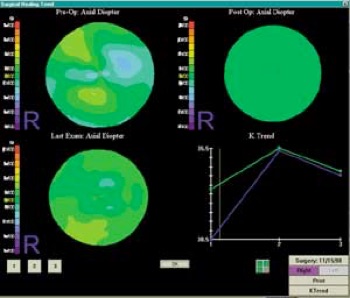
Clinicians use refractive maps to evaluate visual performance in post-refractive surgery patients. This view identifies central islands in patients who have undergone PRK or LASIK. Scaling is another important consideration with corneal topography. In most topographers, the user can utilize the auto-size or normalized scale (relative scale). This strategy essentially subdivides the cornea into dioptric intervals based on its actual curvature range (usually a 6.00D range). Recognize that the actual colors are not specific to a dioptric value when using the normalized scale, but rather are relative to that particular patient's eye.
By contrast, the absolute or standard scale assigns a specific color to each dioptric value and constrains the data to fit within that range. This strategy allows you to directly compare images from different eyes or from significant curvature changes in one eye (e.g., pre- vs. postoperative refractive surgery status). The downside to using the standard scale is that the dioptric range is greatly expanded; hence, clinically significant irregularities may become somewhat obscured when comparing eyes with very different curvature readings. Clinically, it is probably best to use normalized (relative) maps when evaluating one particular eye, and use standard maps when comparing two different eyes or comparing the same eye over time.
Clinical Indications
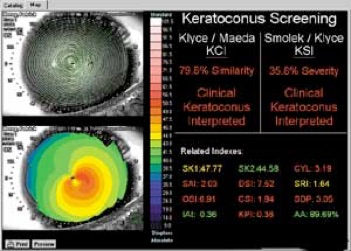
Topography may be indicated in many clinical situations. Conditions such as keratoconus and pellucid marginal degeneration may exhibit corneal steepening before any biomicroscopic signs are evident. In keratoconus, the color maps provide information of the location, size and curvature of the cone's apex, and can help you follow the progression of the disease.
Topography also is invaluable when evaluating pre- and postsurgical patients, particularly those who have had penetrating keratoplasty, radial keratotomy or LASIK. Preoperatively, corneal maps give insight into potential obstacles, such as scarring or irregular astigmatism. Postoperatively, topography can help follow the healing phase and assist with contact lens fitting.
Finally, corneal topography may lend insight into those unusual or difficult refractive cases. Patients with high corneal cylinder often pose a significant challenge when performing retinoscopy and/or auto-refraction, as well as standard keratometry. The topographer is just one more tool that can help you obtain valuable information in assessing refractive error.
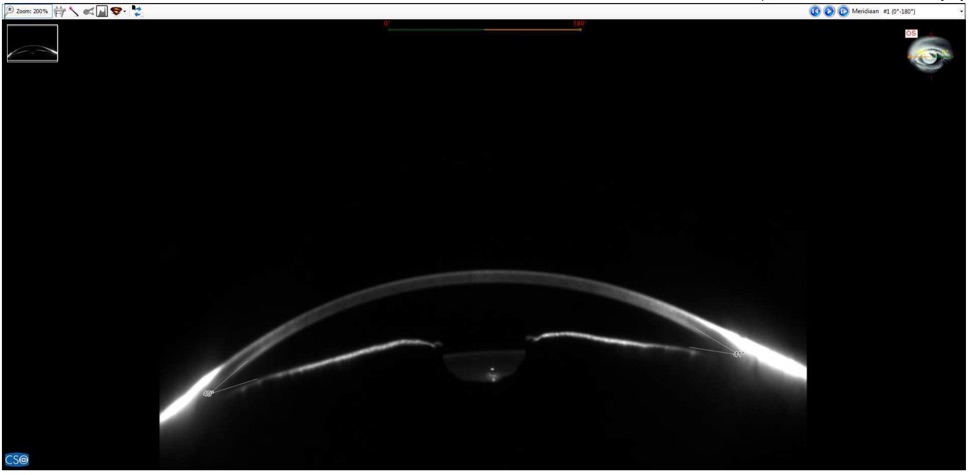
The most profitable and practical use of corneal topography in clinical practice is seen in the fitting of gas permeable lenses. Corneal topography is also useful for annually evaluating the topographical impact of corneal changes in soft contact lens patients.
It is also virtually mandatory in corneal reshaping (Corneal Refractive Therapy or orthokeratology) to monitor the corneal changes occurring as well as the lens positioning from overnight wear.
Most corneal topographers provide software that can design an appropriate contact lens based upon the topography. They recommend lens material, size, design, and even simulate a fluorescein pattern. You can manually alter diameter; base curve and edge design and observe the impact on the simulated pattern. There are even bitoric fitting programs designed for highly astigmatic patients.
This software can greatly simplify the gas permeable fitting process, reduce chair time and increase patient satisfaction.
When considering contact lens correction for these corneal conditions, corneal topography is practically mandatory:
• Post-penetrating keratoplasty, which often results in high or irregular corneal astigmatism;
• Post-RK or LASIK, in which the central cornea flattens relative to the periphery, potentially resulting in residual refractive error and irregular astigmatism;
-
• Advanced keratoconus, in which the central and peripheral curves of the lens are critical to accommodate the protruding cone.
De Lairessestraat 59 1071 NT Amsterdam 020-679 71 55 omca@me.com www.omca.nl
Amsterdam


Amsterdam Eye Hospital
Oogziekenhuis Amsterdam

