EFFECTS OF GLAUCOMA ON OCULAR STRUCTURES
Optic Nerve
The only disc change that is completely diagnostic of glaucomatous damage is progressive thinning of the neural rim.
Typically, progressive glaucomatous neuroretinal loss occurs in a sectorial sequence, usually beginning in the inferotemporal disc quadrant and progressing to the superotemporal, the temporal horizontal, the inferonasal and finally, the superonasal sector.
The size range for a normal optic nerve head is between 1.33 to 2.66 mm in diameter, with 1.5 mm considered to be average. Because the scleral canal size determines disc size, a larger scleral canal results in a larger optic nerve head size.
There are about 1.2 million neurons entering the optic nerve head and these neurons require the same surface area as they leave the eye regardless of the disc size.
Thus, an anatomically large disc creates a physiologically large cup, due to the larger space left over as the neurons leave the retina in the rim tissue.
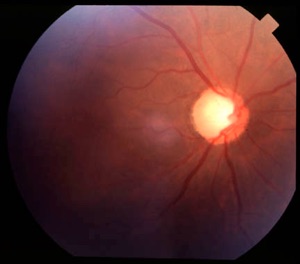
Up to a point, the size of the cup reflects the size of the disc and might not indicate any specific risk of glaucoma. Blacks and Latinos tend to have larger optic nerve head sizes than Caucasians and thus have larger physiological cups.
When examining a patient for the first time, making a cup/disc (c/d) ratio estimation is appropriate. If no information about the patient's c/d ratio history is available, it cannot be determined whether the cup is enlarging, and thus no information about the risk of glaucoma in that eye is available.
However, evaluation of the rim tissue will give a much better index of glaucoma "suspicion." In normal discs, the thickness of the neural rim follows the "ISN'T" rule. The inferior rim is the thickest, followed by the superior rim, the nasal rim, and the temporal rim in order of decreasing thickness.
Typically, the first change in rim tissue caused by glaucoma is thinning of the inferior or the superior rim. Therefore, if the inferior rim is thinner than the superior rim, the patient may have glaucoma and further testing is warranted.
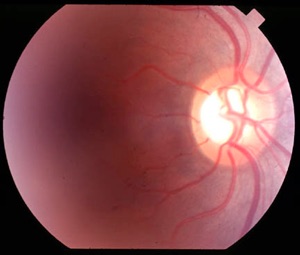
Physiologically large optic nerve cup. The rim thickness follows the "ISN'T" rule and the patient does not have glaucoma.
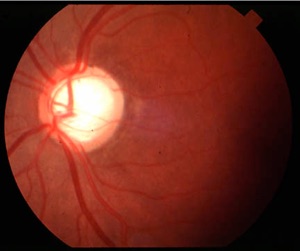
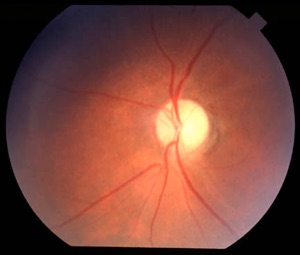
Large optic disc cup. The inferior and superior rim have the same thickness as the temporal rim. This patient has advanced glaucoma.
Typically, the horizontal ratio (H) is compared to the vertical ratio (V), (e.g., H/V = 0.6/0.65), and, in a normal disc, the ratios are very similar.
As indicated above, the first changes to the disc in glaucoma are thinning of the inferior or superior rim followed by thinning of the opposite rim.
This leads to vertical elongation of the cup and a greater vertical than horizontal ratio. A very focal area of thinning is called notching of the rim tissue and is a key sign that glaucoma may be present.
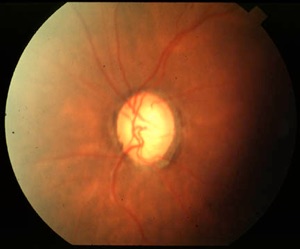
Vertical elongation of the cup due to extensive inferior notching. Also note the peripapillary atrophy.
After superior and inferior rim thinning, temporal thinning of the neuroretinal rim occurs. A temporal rim that is less than 1/8 of the diameter of the optic nerve may indicate glaucomatous excavation.
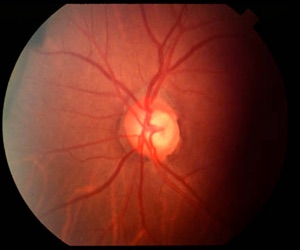
Temporal thinning of the neuroretinal rim tissue. Note the atrophy as well.
Eventually undermining of the neuroretinal rim may extend concentrically around the optic nerve, creating a ‘bean pot’ appearance with deep (1 mm or 3 diopters) cupping. Laminar dots at the base of the cup may also become elongated slits (laminate striae), especially in the superior and inferior areas, as excavation of the nerve head progresses. Eventually only a sliver of nasal rim tissue may remain, with the cup taking up the rest of the nerve head.
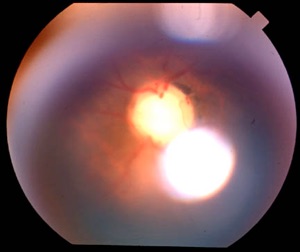
Glaucomatous progression. Upper – advanced glaucomatous cupping. Note the inferior and superior notching. Lower – End-stage glaucoma, with minimal rim tissue.
Depigmentation of the peripapillary region and peripapillary chorio-retinal atrophy may be associated with glaucoma. This sign is called alpha and beta atrophy. It is important to distinguish high myopic atrophy, malinserted discs, and normal variations from peripapillary atrophy associated with glaucoma.
It should be noted that certain optic nerve conditions may mimic glaucoma or be present along with glaucoma.
Examples are cases of ischemic optic neuropathy, toxic neuropathy due to tobacco or alcohol, or retrograde damage of axons due to pathway lesion in the brain (e.g., pituitary adenoma).
Pallor of the nerve heads can be a normal variation (mild temporal pallor) or can be caused by ischemic problems or retinal disease (e.g., retinitis pigmentosa).
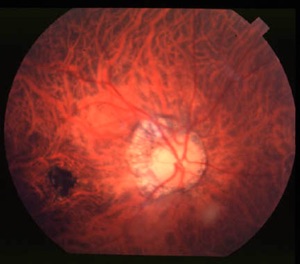
Examples of glaucoma ‘mimickers.’ Upper– myopic peripapillary atrophy. Note the associated Fuch’s spot at the macula. Lower – pallor from ischemic optic neuropathy.
De Lairessestraat 59 1071 NT Amsterdam 020-679 71 55 omca@me.com www.omca.nl

Amsterdam Eye Hospital
Oogziekenhuis Amsterdam

