Introduction
Mooren's ulcer, also referred to as Mooren ulcer, is a rare, painful, inflammatory condition affecting one or both eyes that results in the destruction of corneal tissue.
The intensity of the disease can vary from mild damage to the edges of the cornea in one eye that responds quickly to therapy, to a blinding condition that results in severe damage to both eyes.
History
Mooren's ulcer was first described by Bowman in 1849 and later reported by Mooren in 1867. In the 1960's there was a renewed interest in this condition with many reports coming from developing countries.
Disease Course
Pain is almost always associated with the onset of Mooren's ulcer. One or both eyes may be involved at either the same time or one following the other. Approximately two thirds of cases affect one eye only.
Mooren's ulcer is more common in men than women.
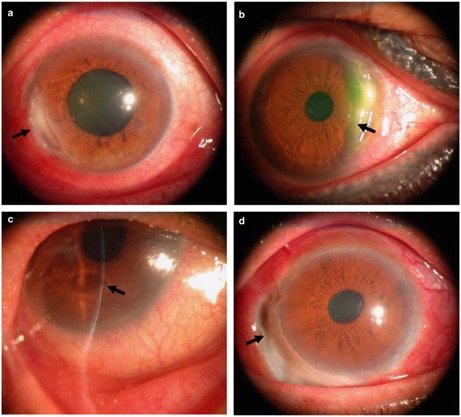
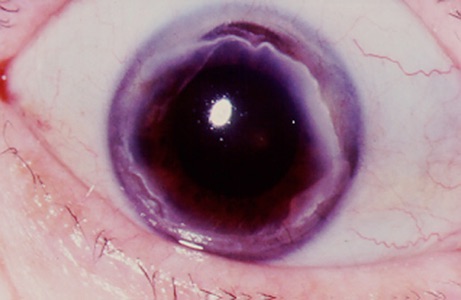
The eye is usually red and the vision may or may not be reduced. Damage begins at the edge of the cornea (near the junction between the white part of the eye and the clear front portion, or cornea) and may progress to involve the central cornea.
A serious complication of Mooren's ulcer is formation of a perforation or hole, in the cornea. If this occurs there is a risk of damage to the sensitive internal structures of the eye and development of a destructive infection inside the eye. In addition, if the center of the cornea is scarred or distorted, light may not be properly focused on the retina and vision will be reduced.
Diagnosis and Testing
There is no specific test at this time for Mooren's ulcer. Instead, testing attempts to rule out other conditions that can cause similar eye problems such as rheumatoid arthritis, systemic lupus erythematosus or Wegener's granulomatosis. Blood tests and a chest X-ray may be ordered. Sometimes, corneal infections can mimic the findings of Mooren's ulcer and therefore testing the cornea for the presence of microorganisms (germs) may be performed. An ophthalmologist makes the diagnosis of Mooren's ulcer once he is convinced that a patient's eye has changes that are characteristic of Mooren's ulcer and that conditions which can mimic Mooren's ulcer have been excluded.
Treatment
In the last 100 years, many treatments have been advocated for Mooren's ulcer.
Currently, most ophthalmologists treat Mooren's ulcer with medications that suppress the immune system.
In mild cases, this may be application of corticosteroid drops to the eye, but in more severe cases, corticosteroids may be administrated by mouth, or intravenously. If the ulceration is not controlled, stronger immunosuppressive medications such as cyclophosphamide may be required.
Surgery is sometimes performed on patients with Mooren's ulcer. A conjunctival resection may be helpful in reducing corneal inflammation and ulceration. Additionally, surgery may be required in patients who develop a perforation or hole in the cornea, to close the hole.
Cause of Condition
The cause of Mooren's ulcer is unknown. It is generally agreed that it is an autoimmune condition in which the patient's own immune system is mistakenly triggered to attack the cornea.
No one knows what this trigger is, but suggestions have included prior eye surgery, prior eye trauma and a variety of infections.
Prognosis
Mooren's ulcer can range from mild cases affecting one eye that do not threaten vision to severe cases involving both eyes and threatening the vision. Because Mooren's ulcer is rare, detailed knowledge is not available which allows prediction of the severity of this disease in a particular patient. Some studies have tried to correlate gender, age, and race with outcomes, but there have been no large studies to confirm these reports.
Research and Future Outlook
Most research on Mooren's ulcer attempts understanding what factors may trigger its development and what proteins are targeted in the cornea.


De Lairessestraat 59 1071 NT Amsterdam 020-679 71 55 omca@me.com www.omca.nl
Amsterdam

Amsterdam Eye Hospital
Oogziekenhuis Amsterdam

