Similar Effects of Selective Laser Trabeculoplasty and Prostaglandin Analogs on the Permeability of Cultured Schlemm Canal Cells
-
1Jorge A. Alvarado<img alt="Corresponding author contact information" src="http://origin-cdn.els-cdn.com/sd/entities/REcor.gif">, <img src="http://origin-cdn.els-cdn.com/sd/entities/REemail.gif" alt="E-mail the corresponding author"> , Rumiko Iguchi, Juan Martinez, Sheetal Trivedi, Amde Selassie Shifera

-
2Beckman Vision Center, Department of Ophthalmology, University of California, San Francisco, San Francisco, California
Purpose
To evaluate whether selective laser trabeculoplasty and prostaglandin analogs regulate the permeability of cultured human Schlemm canal cells by inducing intercellular junction disassembly.
Design
Laboratory investigation.
Methods
Intercellular junctions were made visible in living cells by making them fluoresce after transfection with a plasmid expressing the zonula occludens 1 protein tagged with green fluorescent protein. Schlemm canal cells were treated by direct laser irradiation; by exposure to media conditioned by either lasered Schlemm canal cells or trabecular meshwork cells; by exposure to the prostaglandin analogs latanoprost, bimatoprost, and travoprost; or by the addition of the nonprostaglandin agents brimonidine, timolol, and dorzolamide. Junction disassembly was monitored using fluorescence microscopy, and permeability alterations were measured as changes in conductivity using flow meters.
Results
The direct laser irradiation of Schlemm canal cells caused a 3-fold increase in conductivity. Exposure of the cells to media conditioned by lasered Schlemm canal cells or trabecular meshwork cells induced junction disassembly and a 2- to 4-fold increase in conductivity. Exposure to prostaglandin analogs also induced junction disassembly and a 4- to 16-fold increase in conductivity, whereas the 3 nonprostaglandin agents tested were ineffective in both regards.
Conclusions
Exposure to factors secreted by lasered Schlemm canal cells and lasered trabecular meshwork cells and the application of prostaglandin analogs induced junction disassembly while increasing the permeability of Schlemm canal cells. These findings support our hypothesis that selective laser trabeculoplasty and prostaglandin analogs share a common mechanism that likely mediates their pressure-lowering effects.
FIGURE 1.
Comparison of the differences in the intercellular junction appearance in (Left) Madin-Darby canine kidney (MDCK) cells and (Right) Schlemm canal cells. Junction protein zonula occludens-1 (ZO-1) tagged with green fluorescent protein (GFP; GFP–ZO-1) expression in living MDCK cells was compared with Schlemm canal cells. The cells were transfected transiently with a plasmid construct coding the gene for the junctional protein ZO-1 tagged with the fluorescent protein GFP (×40 magnification).
FIGURE 2.
Junction disassembly process in Schlemm canal cells treated with ethacrynic acid. Ethacrynic acid (0.8 mM) was added to the culture medium and the junction disassembly process of Schlemm canal cells was documented continuously during a 40-minute time-lapse confocal microscopy session.
Snapshots depicting the disassembly process were obtained at (Top left) 0 minutes, (Top right) 22 minutes, (Bottom left) 32 minutes, and (Bottom right) 37 minutes during the experimental period (×40 magnification).

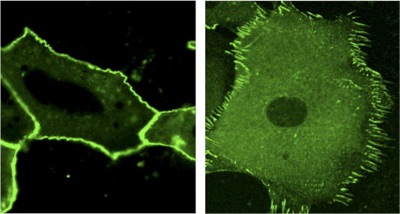
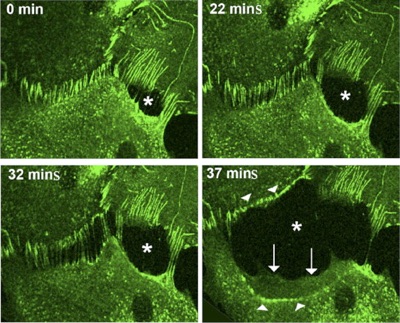
FIGURE 3.
Effects of selective laser irradiation on the barrier property of Schlemm canal cells. Medium conditioned by lasered trabecular meshwork cells was added to Schlemm canal cell cultures, and the cells were incubated for up to 48 hours to monitor the response of the Schlemm canal cellular barrier.
The (Top left) untreated control was compared with the response at (Top right) 24 hours and (Middle left and Middle right) 48 hours in treated preparations (Top left, Top right, and Middle left, ×40 magnification; Middle right, showing a portion of the view enclosed by a rectangle in the Middle left, ×63 magnification). (Bottom) Bar graph showing the effects of direct lasering or treatment with media conditioned by lasered trabecular meshwork cells and lasered Schlemm canal cells for 36 hours on the conductivity of Schlemm canal cells. SC = Schlemm canal; TM = trabecular meshwork.
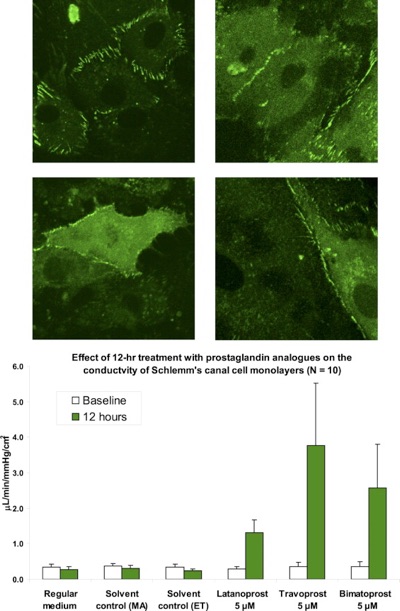
FIGURE 4.
The addition of prostaglandin analogs has direct effects on the junctions and barrier property of Schlemm canal cells. Schlemm canal cells transfected with the junction protein zonula occludens-1 (ZO-1) tagged with green fluorescent protein (GFP; GFP–ZO-1) plasmid were examined by time-lapse confocal microscopy after treatment with prostaglandin analogs for 30 hours. (Top left)
The normal appearance of filopodia and the square shape of Schlemm canal cells in nontreated preparations are shown.
The elongated appearance and the absence of filopodia are shown in preparations exposed to (Top right) latanoprost, (Middle left) travoprost, or (Middle right) bimatoprost for 30 hours (×40 magnification). (Bottom) Bar graph showing the conductivity of Schlemm canal cell monolayers was measured at baseline and after treatment with latanoprost, travoprost, or bimatoprost for 12 hours.
Control samples were treated with regular medium alone or with regular medium to which the appropriate solvent was added at a volume equivalent to that added to the experimental samples. ET = ethanol for travoprost and bimatoprost; MA = methyl acetate for latanoprost.
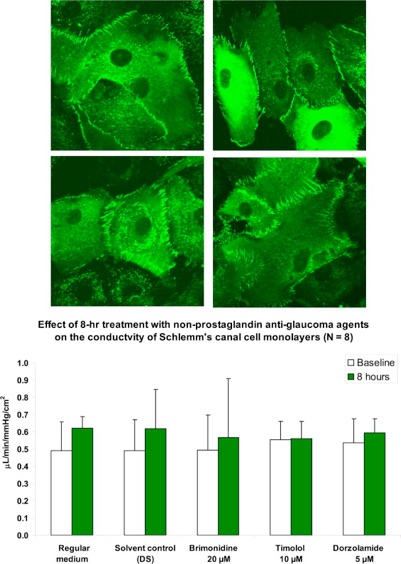

FIGURE 5.
The separate addition of brimonidine, timolol, or dorzolamide has no effect on the junctions and barrier property of Schlemm canal cells.
The results of confocal microscopic studies on intercellular junctions of Schlemm canal cells in (Top left) control samples and in samples exposed for 8 hours to (Top right) brimonidine, (Middle left) timolol, or (Middle right) dorzolamide are depicted.
As shown in these panels, there were no discernable differences in the filopodial status and the cell shape after treatment with brimonidine, timolol or dorzolamide (×40 magnification).
(Bottom) Graph showing the conductivity of Schlemm canal cell monolayers measured at baseline and after treatment with brimonidine, timolol, or dorzolamide for 8 hours.
Control samples were treated with the appropriate solvent added at a volume equivalent to that added to the experimental samples. Solvent was dimethyl sulfoxide (DS), for brimonidine and regular medium for timolol and dorzolamide
FIGURE 6.
Conceptual model showing proposed sites of action of selective laser trabeculoplasty and prostaglandin analogs on the cells present in the conventional aqueous outflow pathway.
The zigzag arrows indicate selective laser trabeculoplasty. The yellow circles represent cytokines, which interact with their receptors on Schlemm canal cells.
De Lairessestraat 59 1071 NT Amsterdam 020-679 71 55 omca@me.com www.omca.nl


Amsterdam Eye Hospital
Oogziekenhuis Amsterdam


